Keratoconus is an eye condition characterised by the thinning and bulging of the cornea, the clear, dome-shaped outer surface of the eye that covers the iris and pupil. In a healthy eye, the cornea maintains a smooth, round shape, allowing light to enter the eye and focus properly on the retina. However, in keratoconus, the cornea gradually becomes thinner and weaker, leading to a cone-like protrusion and irregular shape.
COMMON SYMPTOMS
How Is It Diagnosed?
Keratoconus is diagnosed through a comprehensive eye examination conducted by an eye care professional, typically an optometrist or ophthalmologist. The diagnostic process may involve several tests and procedures to evaluate the shape, thickness, and overall health of the cornea. Here are the common steps involved in diagnosing keratoconus:
- Patient History: Gather information on symptoms, family history, and previous eye issues
- Visual Acuity Testing: Assess vision clarity
- Refraction Test: Measure refractive error for glasses or contact lens prescription
- Corneal Topography: Map cornea shape to detect irregularities indicative of keratoconus
- Corneal Pachymetry: Measure corneal thickness; thin corneas may suggest keratoconus
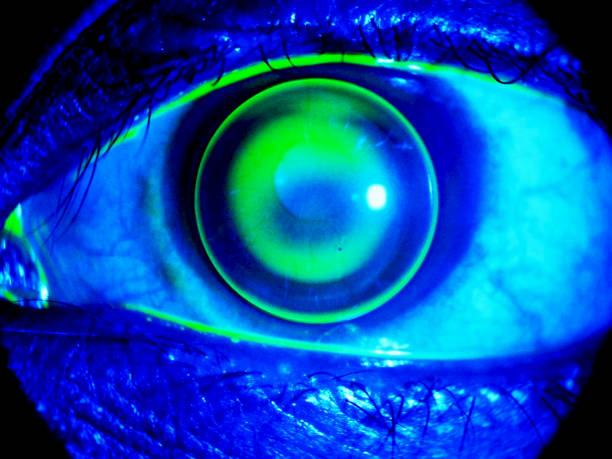
- Slit-Lamp Examination: Examine cornea and eye structures for abnormalities
Treatment Options
There are several treatment options available for keratoconus, ranging from non-surgical approaches to surgical interventions. The choice of treatment depends on the severity of the condition, the progression of keratoconus, and individual factors such as age, corneal thickness, and visual needs. Here are the common non-surgical and surgical treatment options for keratoconus:
NON-SURGICAL
SURGICAL
Contact us today to book an appointment if you are experiencing concerns with your vision. We are here to help address any issues and provide solutions tailored to your individual needs. Our knowledgeable optometrists will conduct a comprehensive evaluation, discuss your treatment options, and develop a tailored plan to address your unique needs and goals.



